STELLATE GANGLION BLOCKS AND RFA
Indications
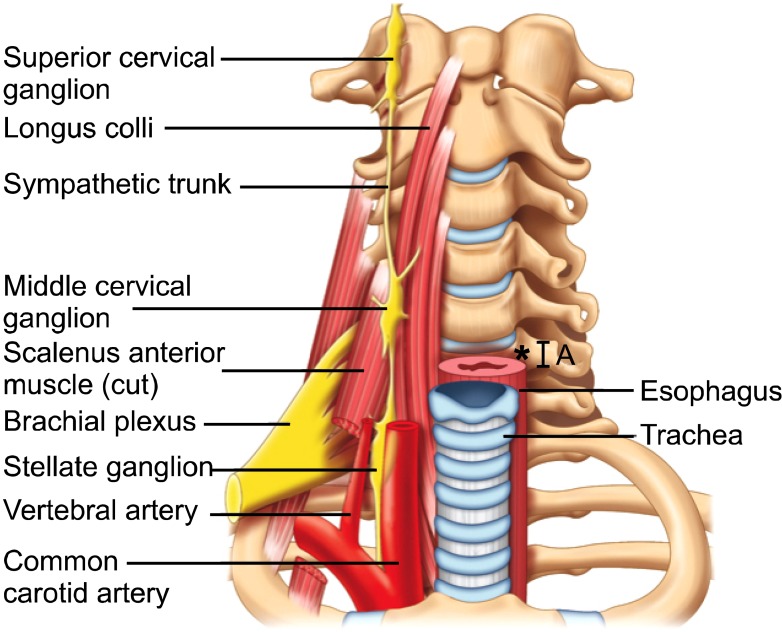
A stellate ganglion block (sympathetic block) is an injection of local anesthetic into the front of the neck. It is typically ordered by your doctor for pain located in the head, neck, chest or arm that is caused by sympathetically maintained pain
- Complex Regional Pain Syndrome (CRPS I), also known as Reflex Sympathetic Dystrophy (RSD) and CRPS II also called causalgia , is a condition involving chronic, intense pain that usually occurs in the arms, hands, legs or feet. It is thought that CRPS is precipitated by trauma to nerves in the affected area or an immune reaction. In addition to allodynia, hyperalgesia, and central sensitization, CRPS patients may experience changes in skin texture, color and temperature, and reduced range of motion in affected extremities. There are two types of CRPS: CRPS 1 is a chronic nerve disorder that occurs in an extremity after a minor injury, and CRPS 2 is caused by direct injury to a nerve. The International Association for the Study of Pain supports the use of sympathetic blocks to reduce sympathetic nervous system over-activity and other symptoms in CRPS patients, and educational reviews promote stellate ganglion blockade as beneficial in such individuals
- Herpes zoster (shingles)
- Intractable angina.
- Circulation problems, particularly Raynaud's
- Shoulder-hand syndrome – Stellate ganglion block can be used to treat this chronic, incompletely understood condition of the shoulder and arm which involves intractable pain, limited joint motion, swelling of the upper extremities, muscle fibrosis and atrophy, and bone decalcification
- Facial pain – Pain felt in the face may be caused by a nerve disorder, an injury, or an infection
- Phantom limb pain – Phantom limb pain is pain that is felt in the area where an extremity has been amputated
- Scleroderma and secondary raynauds
- Craniofacial hyperhidrosis
- Hot flashes – Stellate ganglion blocks may help control the hot flashes caused by menopause and other reasons, as well as related sleep dysfunction.
Procedure
After you sign a consent form and your blood pressure is checked, an intravenous will be started. Skin temperature monitors will be placed on both of your hands. You will be asked what your pain score is on a scale of 0 to 10. The procedure will be done with you lying on your back with a sheet rolled up between your shoulder blades. Your neck will be cleaned with an antiseptic.
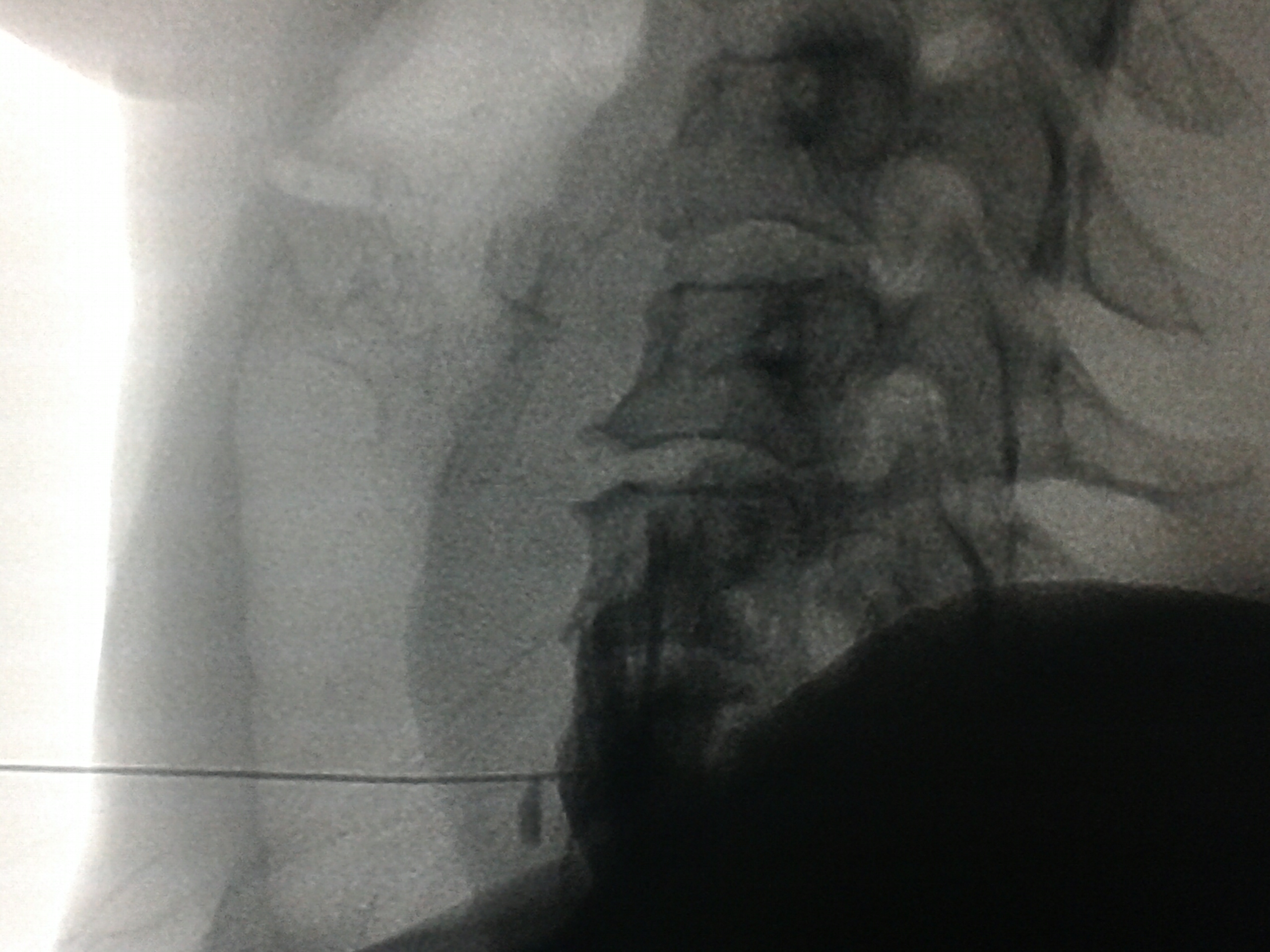
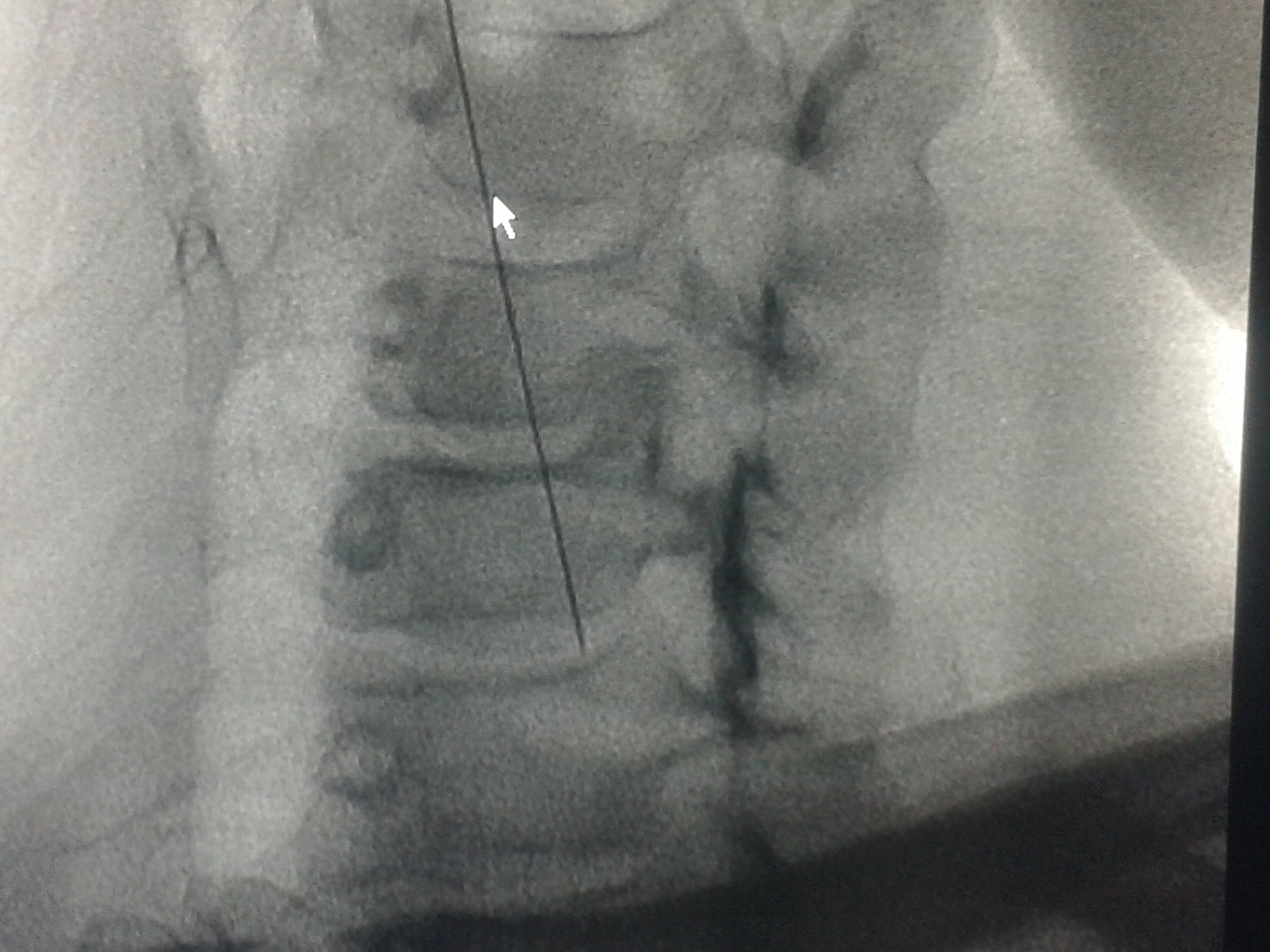
Generally, the patient will be given intravenous (IV) sedation to promote comfort during the procedure. The physician uses painless fluoroscopy to help visualize the area being injected. Fluoroscopy is an x-ray imaging technique that provides real-time, live images of the internal structures of a patient through the use of an x-ray source and fluorescent screen. When the needle is in the correct place, the medicine (local anesthetic) is injected through the needle. The needle is then removed and the procedure is complete. This usually takes about 5 to 10 minutes. If your pain is usually in your head, you will remain lying down. If your pain is usually in your arm, you will be asked to sit up so the medicine spreads down. The medicine can take 10 to 20 minutes to take full effect. You will be watched during that time. Your doctor will be checking to see if the expected changes take place, as well as to see what effect, if any, there is on your pain. You will be observed for 15 to 20 minutes. Your pulse and blood pressure will be monitored during this time. Your intravenous will be removed, and you will be discharged when you are ready and your ride is present. You may have some local tenderness from the needle, which ice will help relieve. You can also resume taking your normal pain medications.
Special Instructions
This procedure cannot be performed if you have an active infection (and are on antibiotics), flu, fever, extremely high blood pressure, or if you are on blood thinners (e.g., aspirin, Coumadin, Plavix, Pletal). Blood thinners must be stopped five to seven days prior to the procedure. For your safety, please inform us if any of these conditions exists.
Side Effects And Complications
The risks of the procedure-though rare-include seizure (if the medication is injected into a blood vessel), pneumothorax (collapsed lung), brachial plexus block , spinal or epidural block , allergy to the medication used, nerve damage and bruising at the injection site.
There are some expected changes that result from blocking the sympathetic nerves. These changes last for the life of the local anesthetic (approximately four to six hours). They include drooping of the eyelid, "bloodshot eye," a stuffy nose, and a temperature increase on the injected side. You may also experience hoarseness.
Procedures
- EPIDURAL STEROID BLOCK ( TFESI, CAUDAL, INTERLAMINAR )
- CERVICAL EPIDURAL NEUROPLASTY
- INTRAARTICULAR FACET BLOCKS
- MEDIAL BRANCH RFA FOR FACETOGENIC PAIN
- THIRD OCCIPITAL NERVE BLOCKS AND RFA
- C0-C1 and C1-C2 BLOCKS
- OCCIPITAL NERVE BLOCKS AND RFA
- SACROILIAC JOINT BLOCKS and RFA
- GASSERIAN RFA FOR TRIGEMINAL NEURALGIA
- BALLOON COMPRESSION FOR TRIGEMINAL NEURALGIA
- INTRAARTICULAR SHOULDER PROCEDURES
- PROLOTHERAPY
- PRP THERAPY
- GENICULAR NERVE RFA FOR KNEE PAIN
- LUMBAR SYMPATHECTOMY FOR LOWER LIMB ISCHEMIA & CRPS
- T2-T3 GANGLION NEUROLYSIS FOR UPPER LIMB ISCHEMIA AND CRPS
- STELLATE GANGLION BLOCKS AND RFA
- TRIGGER POINT INJECTIONS
- INTRARTICULAR TMJ PROLOTHERAPY
- KNEE JOINT INJECTIONS INCLUDING VISCOSUPPLEMENTATION
- CELIAC PLEXUS BLOCKS AND NEUROLYSIS
- SUPERIOR HYPOGASTRIC PLEXUS BLOCKS AND NEUROLYSIS
- GANGLION IMPAR BLOCK AND RFA