Low Back Pain
Low back pain (LBP) is an extremely common problem that affects at least 80 percent of the population at some point in their lifetime. Back pain or backache is the leading cause of occupational disability and the most common cause of missed workdays. As the population ages and our lives become more sedentary, this situation is unlikely to change. Low back pain affects men and women equally. About 20 percent of people affected by acute low back pain go on to develop chronic low back pain lasting a year or more. Although once thought to be a very short-lived, recent studies have shown that nearly 75% of these acute low back pain patients continue to suffer from pain at 3 months, with no significant improvement at 12 months.

Contributory Factors
Biophysical: Structural changes and impaired stabilisation of lumbar muscles. Psychological: Anxiety, Depression. Social: Low income, education levels, and work satisfaction. Lifestyle: High body mass index, smoking, low levels of physical activity.
Causes
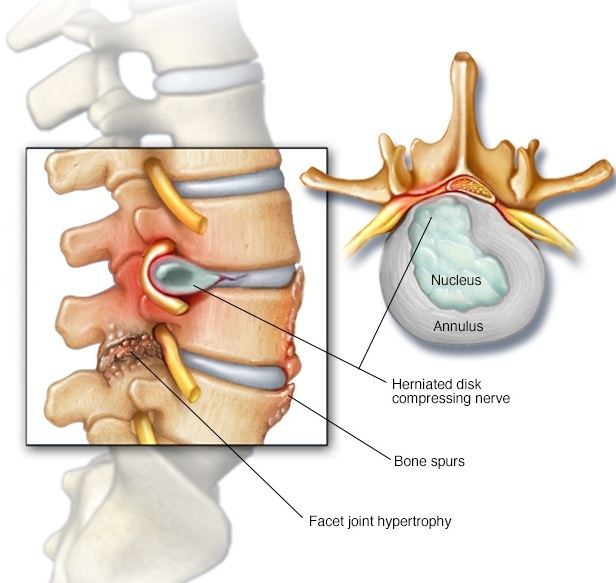
A) Mechanical (80-90%) Myofacial Low back pain - usually attributed to muscle strain or ligament injury 65-70%. Facet athropathy: It is caused by the degeneration or trauma to the synovial joints present in the back. Pain is mostly axial with some radicular component. Pain aggravates on extention and turning twisting movements. Mostly seen in older individuals. There is localized tenderness in para spinal region. Spondylosis term is used is a degenerative condition that may worsen as a person grows older. It can affect any region of the spine. Spondylosis can affect the spine's intervertebral discs (eg, degenerative disc disease) and facet joints. Sacroiliac joint Dysfunction: Sacroiliac (SI) joint pain is felt in the low back and buttocks. The pain is caused by damage or injury to the joint between the spine and hip. Sacroiliac pain can mimic other conditions, such as a herniated disc or hip problem. Vertebral fracture: A compression fracture is typically caused by a loss of bone mass (osteoporosis) that occurs as part of ageing. A fall, a cough or lifting a heavy object may cause a fracture of the back bones. Congenital deformity (such as scoliosis, kyphosis, transitional vertebrae. B) Neurogenic(5-15%) Herniated disc. Spinal stenosis: Lumbar spinal stenosis is caused by insufficient room in the spinal canal for the neural elements. It is mostly degenerative in origin. Patients with spinal stenosis experience leg pain with prolonged standing or walkingóthe classic syndrome of neurogenic claudication. Annular fissure with chemical irritation of nerve root or Discogenic low back pain: Its causes radicular LBP or sciatica. It happens when the nucleus inside the disc bulges or leaks through the annular tear causing indentation of thecal sac or chemical neuritis of Dorsal Root Ganglia (DRG) or mechanical compression of the nerve roots coming out of spinal canal. Failed back surgery syndrome (such as arachnoiditis, epidural adhesions, recurrent herniation); may cause mechanical back pain as well. C) Non-Mechanical spinal conditions (1-2%) Neoplastic (such as primary or metastatic) disease. Infection (such as osteomyelitis, discitis, abscess). Inflammatory arthritis or spondyloarthritis: They share certain clinical characteristics (eg, back pain, uveitis, GI symptoms, rashes). Some are strongly associated with the HLA-B27 allele. Clinical and genetic similarities suggest that they also share similar causes or pathophysiologies. Rheumatoid factor (RF) is usually negative in the spondyloarthropathies (hence, why they are called seronegative spondyloarthropathies). They include ankylosing spondylitis, reactive arthritis, psoriatic arthritis, and other disorders. D) Others (2-4%) Fibromyalgia. Somatoform disorder (such as somatization disorder, pain disorder). Malingering. Radicular symptoms may result from either chemical mediators released from degenerated discs or mechanical irritation. Causes of Spinal canal stenosis include foraminal narrowing, osteophyte formation, spondylolisthesis, post- surgical changes, and congenitally short pedicles.
Clinical Presentation
Signs of nerve root irritation 1. Leg pain greater than back pain. 2. Radiation into foot or lower leg. 3. Numbness and paraesthesias in dermatomal distribution. 4. Diminished leg reflexes. 5. Positive straight leg raising test (L4-S1 nerve roots). 6. Positive femoral stretch test (L2-L4 nerve roots). 7. Leg pain exacerbated by coughing, sneezing, or Valsalva maneuver. Imaging MRI is the investigation of choice for patients suffering from chronic low back pain. Bulging or degenerative discs, annular fissures, tumours, infection all can be seen in MRI and major causes can be ruled out. Dynamic spine X rays are also important esp. to rule out spondylolisthesis.
Treatment
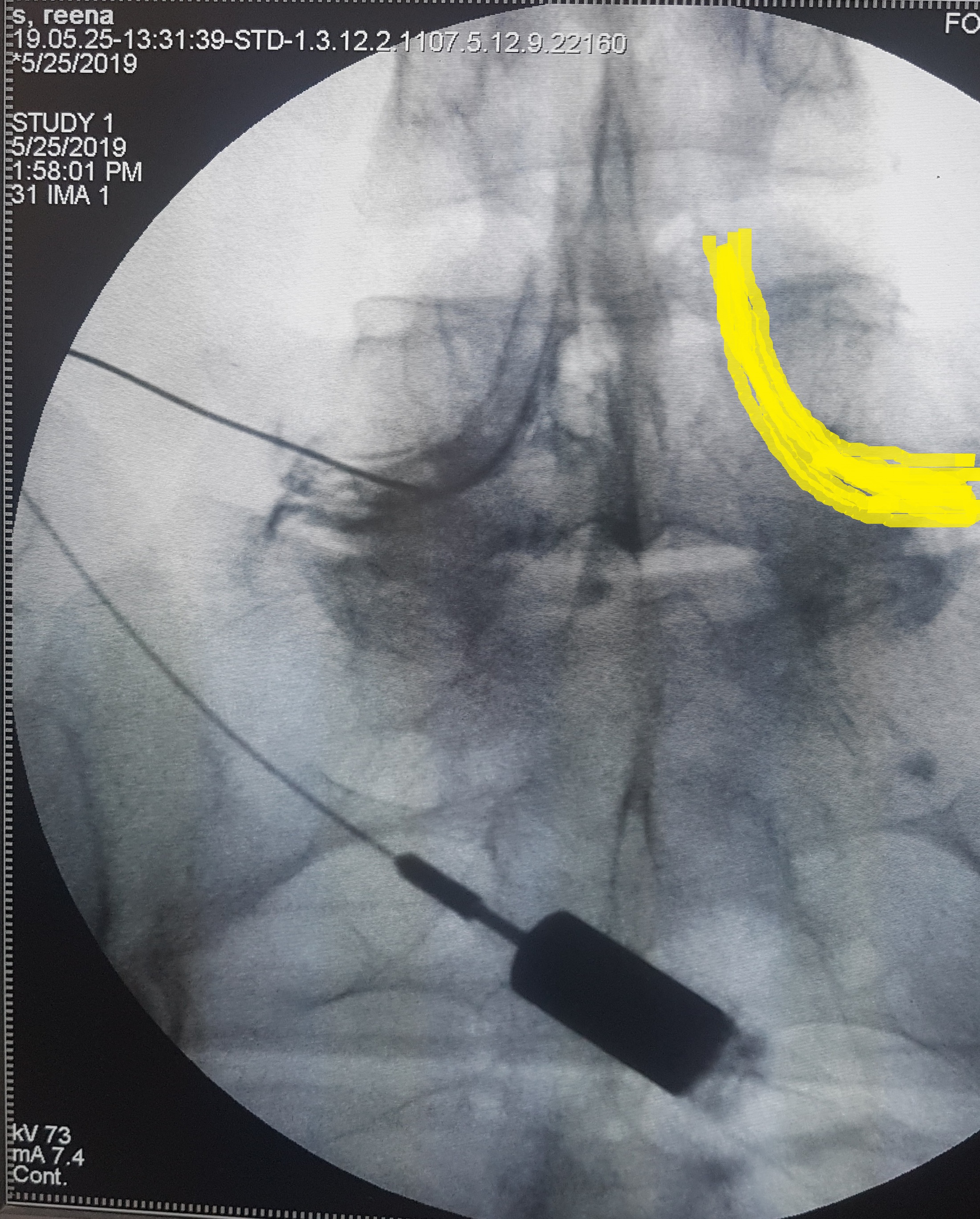
90% of the episodes of low back pain resolves with medications , physiotherapy and back strenghthening exercises. Further diagnostics work up is necessary if there are red flags such as possible fracture, tumor or infection, bladder or bowel dysfunction, severe or progressive neurological dysfunction in the legs or pain not improving on conservative means. When conservative treatment fails, it is important to identify the structures responsible for the generation of low back pain. Newer imaging techniques like MRI have immense value in confirming these diagnoses. NONSURGICAL OPTIONS OF LOW BACK PAIN MANAGEMENT: 1. Transforaminal epidural steroid injections or caudal epidural steroid injection. 2. Vertebroplasty or Kyphoplasty. 3. Intraarticular Sacroiliac joint steroid injection. 4. Sacroiliac Joint prolotherapy. 5. Radiofrequency ablation of Sacroiliac joint nerves. 6. Intraarticular facet steroid injections. 7. Medial branch of Dorsal ramus RFA for Facet arthropathy. 8. Racz catheterization for failed back surgery syndrome. 9. Intradiscal Ozone therapy. Disc Fx. SURGICAL OPTIONS: 1. Microscopic or endoscopic discectomy. 2. Laminectomy and spinal canal decompression. 3. Fusion surgery. 4. Disc replacement.
Types of Pain
- Neck Pain
- Low Back Pain
- Thoracic Spine Pain
- Headache
- Shoulder Pain
- Elbow Pain
- Wrist Pain
- Knee Pain
- Peripheral Vascular Disease
- Neuropathic Pain Syndromes
- Fibromyalgia And Other Myofacial Pain Syndromes
- Chronic Regional Pain Syndrome
- Facial Pain
- Foot Pain
- Abdominal Wall Pain Syndrome
- Sacroiliac Joint Pain
- Cancer Pain
- Urogenital Pain Syndrome
- Chronic Pelvic Pain