Foot Pain
Foot pain refers to any pain or discomfort in one or more parts of the foot, such as the following: toes
heels
arches
soles
The pain can range from mild to severe, and it may last a short time or be an ongoing issue. Many measures can help relieve your foot pain.

Contributory Factors
It is more likely to occur in a person whose lifestyle or occupation causes repetitive impact to the foot. Activities such as running, marching, or dancing may trigger or worsen symptoms. Possible other factors that increase the risk of foot pain include obesity, prolonged standing, and limited ankle flexibility Foot pain occurs more frequently among runners, and, in this group, possible factors that increase the risk include:
- Excessive training (particularly a sudden increase in the distance run)
- Improper running shoes
- Running on unyielding surfaces
- Flat feet
- High arches
Causes
Injury, overuse or conditions causing inflammation involving any of the bones, ligaments or tendons in the foot can cause foot pain. Arthritis is a common cause of foot pain. Injury to the nerves of the feet may result in intense burning pain, numbness or tingling (peripheral neuropathy).
Some common causes of foot pain include:
- Achilles tendinitis
- Achilles tendon rupture
- Bone spurs
- Bunions
- Bursitis (joint inflammation)
- Diabetic neuropathy (nerve damage caused by diabetes)
- Flatfeet
- Gout (arthritis related to excess uric acid)
- Hammertoe and mallet toe
- Metatarsalgia
- Morton's neuroma
- Osteoarthritis (disease causing the breakdown of joints)
- Plantar fasciitis
- Reactive arthritis
- Retrocalcaneal bursitis
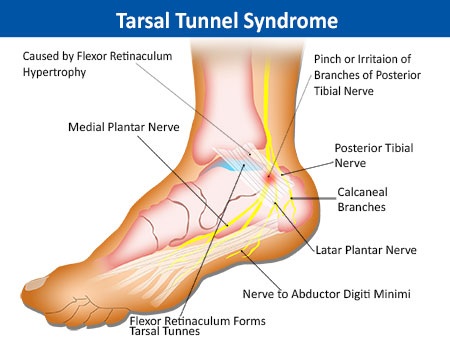
- Tarsal tunnel syndrome
Investigation
- Blood Investigations : If an inflammatory condition is suspected a full blood count, ESR, CRP, rheumatoid screen, antibody screen and HLA serotype may be helpful. We have found these tend to be non-specific and an isotope bone scan is often more helpful.
- Imaging studies play a key role in diagnosis and management. Initial assessment is typically done by plain radiography; however, magnetic resonance imaging has superior soft-tissue contrast resolution and multiplanar capability, which makes it important in the early diagnosis of ambiguous or clinically equivocal cases when initial radiographic findings are inconclusive. Computed tomography displays bony detail in stress fractures, as well as in arthritis and tarsal coalition. Bone scanning and ultra-sonography also are useful tools for diagnosing specific conditions that produce chronic foot pain.
- Nerve conduction testing may occasionally be useful in suspected tarsal tunnel syndrome or the "heel pain triad" of plantar fasciitis, tibialis posterior tendinopathy and tarsal tunnel syndrome.
Treatment
Commonly used treatments for plantar fasciitis include the following:
- Rest : Limiting athletic activities and getting extra rest may help to reduce symptoms. Icing : Applying ice to the area, for example, for 20 minutes up to four times daily, may relieve pain. Ice and massage may also be used before exercise.
- Stretching : Stretching exercises may be helpful. Home exercises include the calf-plantar fascia stretch , foot/ankle circles , toe curls , and toe towel curls . Be sure to perform these exercises with care to avoid causing more pain.
- Analgesics: A clinician may recommend a short course of a nonsteroidal anti-inflammatory drug (NSAID) or opioids such as to relieve pain
- Prosthesis and Protective footwear — Athletic shoes, arch-supporting shoes , or cushion-soled shoes with gel pad inserts or heel cups may provide temporary pain relief. Silicone inserts have been found to provide better support than felt pads or rubber heel cups. Magnetic insoles have not been found to provide any additional benefit.
- Splints may be helpful when worn overnight to position the foot and heel to provide pain relief and a gentle stretch.
- Wearing slippers or going barefoot may cause symptoms to return, even if the floors are carpeted. Thus, the first step out of bed should be made with a supportive shoe or sandal on.
If these noninvasive measures fail to improve the pain, a healthcare provider may recommend one of the following treatments:
- Steroid injection — An injection of a steroid (glucocorticoid) medication may be given into the foot to relieve pain, although the effect may wear off after a few weeks. The injection can be repeated, although many clinicians limit the number of times they will give injections because they believe repeated injections may weaken the tissues of the sole of the foot.
- Prolotherapy is an injection treatment used to initiate a healing response in injured connective tissues such as tendons and ligaments, common in painful foot and toe conditions.
- PRP has also been utilized for treating foot pain. PRP has higher concentrations of substances that encourage your body to grow new tissue. This may help your body do a better job of recovering from certain injuries or conditions. PRP injections may reduce pain and get your muscles moving more smoothly.
- Surgery: Surgery is rarely required for people with plantar fasciitis. It would only be recommended if all other treatments had failed and if the person had persistent symptoms for at least 6 to 12 months
Types of Pain
- Neck Pain
- Low Back Pain
- Thoracic Spine Pain
- Headache
- Shoulder Pain
- Elbow Pain
- Wrist Pain
- Knee Pain
- Peripheral Vascular Disease
- Neuropathic Pain Syndromes
- Fibromyalgia And Other Myofacial Pain Syndromes
- Chronic Regional Pain Syndrome
- Facial Pain
- Foot Pain
- Abdominal Wall Pain Syndrome
- Sacroiliac Joint Pain
- Cancer Pain
- Urogenital Pain Syndrome
- Chronic Pelvic Pain